Author Archive
UT to develop training tool to better care for patients who are homeless
Wednesday, February 13th, 2019The University of Toledo is developing a virtual reality training to improve Ohio Medicaid providers’ cultural competency and reduce implicit bias as a way to better understand the patients they serve. The virtual reality training focuses on the barriers to health care faced by those without stable, permanent housing.
UT faculty from the College of Medicine and Life Sciences and the College of Health and Human Services will conduct interviews and observe interactions in an area homeless shelter to build a realistic portrait of the health-care struggles experienced by individuals who depend on urban homeless shelters for their housing.
From that data, faculty and staff from the College of Medicine and Life Science, the School of Population Health in the College of Health and Human Services and the Interprofessional Immersive Simulation Center will create an interactive experience that will electronically place clinicians into a model homeless shelter as fly-on-the-wall observers.
“There’s a lot of attention nowadays to how one’s background and social structure impact not only their health but also how successful they are in using the health-care system,” said Dr. Lance Dworkin, chair of UT’s Department of Medicine and the primary investigator for the project. “If we understand that, we can integrate that knowledge into the care we provide so it’s more effective.”
The University also is building a robust evaluation component into the program that will monitor physical biomarkers such as heart rate, blood pressure and respiratory rate while participants are engaged in the simulation. Using assessment software developed by Dr. Scott Pappada, assistant professor of anesthesiology and bioengineering, and a co-investigator on the project, researchers will collect data before and after the simulation to learn how the program affects clinicians and whether it helps them connect with individuals who are marginalized by society.
The project is funded by a $1.24 million grant from the Ohio Department of Medicaid.
UT’s work is part of a larger partnership between the Ohio Department of Medicaid and Ohio’s medical schools, administered by the Ohio Colleges of Medicine Government Resource Center. Like many projects managed by GRC, the Medicaid Equity Simulation project is aimed at reducing health disparities, addressing the social determinants of health and improving patient care and health outcomes for Ohio’s Medicaid population.
Over the course of the homeless shelter simulation, health-care providers will see rudimentary sleeping quarters, dining and social areas, observe the interactions between guests and staff and listen in on conversations gleaned from the real-life interviews.
“The big message here is how does one change clinical decision making based on what is learned about an individual in this environment,” said Dr. Shipra Singh, assistant professor of health education and public health and a co-investigator on the project.
Singh, who is directing the scripts that will be used in the simulation, said those changes could be as simple as not forcing someone who has no access to reliable transportation to go to the back of the line if they’re late for an appointment, or understanding that immediate lifestyle changes may not be possible.
“You need to listen to the patient rather than just look at them, and understand the cultural context they’re coming from and what really matters to them,” Singh said.
The program is expected to be ready to launch to Ohio Medicaid providers within The University of Toledo Medical Center in May and disseminated throughout the community by June.
A new mouse model from UT may unlock the secrets of treating Type I diabetes
Tuesday, February 12th, 2019Researchers at The University of Toledo have found a new way to replicate in lab mice the development and progression of Type I diabetes, a breakthrough that has the potential to reshape how the chronic disease is studied.
An estimated 1.25 million Americans are living with Type I diabetes. While the condition can be managed with insulin, finding a treatment or cure for the disease has been elusive — in part because scientists have not had a reliable animal model that mimics the full scope of human Type I diabetes.
“We see these patients every day. We see them come to the hospital, we see how they struggle,” said Dr. Juan Jaume, professor of medicine in UT’s College of Medicine and Life Sciences and senior author of the new invention. “Unfortunately, research has been held back because the scientific community didn’t have a good model to study the disease and its progression. Now we do. We have developed a mouse model that is a step forward toward finding a cure.”

Dr. Shahnawaz Imam, left, and Dr. Juan Jaume display an array of diabetes management tools. A new mouse model developed at the University of Toledo may open the door to research that finds new therapies.
The first peer-reviewed study using the UT-developed mouse model was published Feb. 7 in the natural sciences journal Scientific Reports.
In that study, Jaume, who is also chief of the Division of Endocrinology and director of UT’s Center for Diabetes and Endocrine Research, and co-collaborator Dr. Shahnawaz Imam, a senior researcher in the Departments of Medicine and an associate member of the Center for Diabetes and Endocrine Research, looked at how a certain protein can influence T-cells in the pancreas to delay the onset of diabetes.
While the study adds to the overall knowledge about diabetes, it is the mouse model that holds the real potential.
In the new model, mice spontaneously develop Type I diabetes and, importantly, the full range of complications experienced by diabetes patients. That allows study of the disease and its natural progression in a way not previously possible.
“Our model is showing exactly the same physiopathology that humans with diabetes suffer,” Imam said. “Our mice are getting eye problems, they are getting kidney problems and also neuropathy. That’s a very important part of this — they have the same human complications that all diabetes patients have, not just those with Type I.”
The laboratory mice were developed through a series of selective breeding experiments and genetic modification that included adding human genes to the mice.
A provisional patent on the Spontaneous Type I Diabetes Mouse Model was filed last year.
Type I diabetes, formerly known as juvenile diabetes, results from an autoimmune attack on cells in the pancreas that produce insulin. Without insulin, the body cannot process the sugars in food, leading to dangerously high blood sugar.
Though many species develop diabetes, Jaume said the process of Type I diabetes seems to be unique to humans. And while scientists have frequently used other specially bred mice, including what’s known as the non-obese diabetic mouse, to study diabetes and test treatments, those lab animals don’t mimic the exact human pathophysiology of the disease.
“The existing non-obese diabetic mouse model does not completely resemble the human condition,” Jaume said. “There are more than 125 different therapies that cure Type I diabetes in non-obese diabetic mice. Clinical trials were developed because of that model, but none have worked in humans. Everybody has been searching for a better model.”
Jaume and Imam have been working on their model for more than a decade. It is already showing research promise.
Using the same idea behind CAR T-cell therapy for cancer, in which certain immune system cells are taken from a patient and paired with an artificial receptor that once reintroduced into the body homes in on the tumor, the team is developing cellular therapies for diabetes that uses the mice’s regulatory cells to cool down the immune response.
The University has also filed a provisional patent on the treatment method, and Jaume and Imam will soon begin a more in-depth study of its effectiveness.
UT research looks at fiber as a trigger and cure for inflammatory bowel disease
Tuesday, February 5th, 2019New research from The University of Toledo’s College of Medicine and Life Sciences may give patients suffering from inflammatory bowel disease a better roadmap for managing their symptoms by changing the type of fiber they eat during flare-ups.
Because there’s no cure for the chronic condition, patients living with Crohn’s disease and ulcerative colitis — the two most common types of IBD — often rely on anti-inflammatory or immunosuppressive drugs and careful diet planning to manage their symptoms, said Dr. Matam Vijay-Kumar, the senior author on the study and director of the UT Microbiome Consortium and associate professor in the UT Department of Physiology and Pharmacology.
But even that can seem like guesswork.
“IBD can be a debilitating condition and its prevalence is on the rise. For IBD patients, there has been a puzzling question of why they report poor tolerance to certain types of dietary fibers,” said Dr. Vishal Singh, a Crohn’s and Colitis Foundation Fellow mentored by Vijay-Kumar at UT.
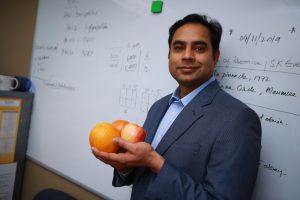
Dr. Vishal Singh, a Crohn’s and Colitis Foundation Fellow at UT, holds apples and oranges, common natural sources of pectin.
“For healthy people, dietary fibers are good,” he said. “But when it comes to the IBD patients, not all natural fibers are created equal, thus their metabolism is distinct. We wanted to understand why.”
In a study published last month in the gastroenterology journal Gut, a team of UT researchers demonstrated a diet rich in pectin or pectin-derived fibers may be a better alternative to the prevailing dietary fiber guidelines aimed at helping patients improve their IBD symptoms.
The study also confirmed that inulin and inulin-like fiber exacerbated colitis in lab mice.
Inulin and pectin are two of the most common refined fibers added to processed foods as a way to add texture and boost their health appeal. Both are indigestible soluble fibers, Vijay-Kumar said, but they require different bacterial enzymes to be broken down in the gut into short-chain fatty acids.
“Many patients try to avoid fiber,” said Singh, the study’s first author. “However, the research shows it’s not about reducing fiber in general but getting the right kind into your system.”
Singh and his fellow researchers said the finding could assist patients in developing a better diet for managing or preventing flare-ups.
“Following strict dietary guidelines is not new for IBD patients. Physicians often recommend patients limit or avoid a group of foods that contain fermentable carbohydrates, commonly known as the low-FODMAP diet,” Vijay-Kumar said. “Pectin is not included in that diet, but our research shows it brings a clear benefit.”

Dr. Matam Vijay-Kumar
The study was supported by the Crohn’s and Colitis Foundation and the National Cancer Institute of the National Institutes of Health.
In the study, researchers examined the role played by bacteria that naturally reside in our guts. They demonstrated that inulin promoted accelerated growth of one particular harmful bacterial strain, while pectin did not.
They also found that a brief period of fasting may boost our body’s production of a physiological inflammation inhibitor that can protect against the inflammatory reaction caused by the gut bacteria processing inulin.
“For me, this study connects very well from bench to bedside,” Singh said. “If an IBD patient is noticing complications after eating some type of food, they can look to see if is rich in inulin or inulin-type fibers. If it is, they can switch to foods enriched with pectin.”
Pectin is found naturally in a variety of foods, including apples. It also can be derived from other natural sources, such as orange peels, and used as a food additive.
Though the study looked only at pectin and inulin, the team hopes to conduct similar studies on a wide variety of dietary fibers present in processed foods with the goal of learning more about how different types of fiber cause or reduce colonic inflammation.
First class of Toledo Fire Department paramedics among new inductees to UT Emergency Medicine Wall of Honor
Monday, February 4th, 2019The University of Toledo will add 14 names to the Emergency Medicine Wall of Honor at the eighth annual induction ceremony on Tuesday, Feb. 5, including the first group of Toledo firefighters to be certified as paramedics.
This year’s other inductees are a long-time clinical nursing educator and an emergency medical services outreach education coordinator.
The ceremony will begin at noon in Collier Building Room 1000B on Health Science Campus with a welcome from UT President Sharon L. Gaber. A reception with light refreshments begins at 11:30 a.m.
Dr. Kristopher Brickman, professor and senior associate dean for innovation in the College of Medicine and Life Sciences, and Dr. Christopher Cooper, executive vice president for clinical affairs and dean of the College of Medicine and Life Sciences, also are scheduled to give remarks.
“This award recognizes people who have been instrumental in developing and defining what emergency care is in our region,” Brickman said. “We want to honor some of our unsung heroes of emergency medicine who have helped save lives and made a real difference in our community.”
The Emergency Medicine Wall of Honor, made possible through funding from IPI Insta-Plak Inc. and The Blade, was established in 2011 to celebrate the achievements of those who are committed to service within the emergency medicine community.
Each year, nominations are submitted by a committee of community stakeholders and reviewed by a multidisciplinary selection committee. This year’s group is larger because of the inclusion of all 12 members of the Toledo Fire Department’s first paramedic class.
“Those firefighters were a unique group of people who basically were out there doing something that nobody else had done before,” Brickman said. “For our region they were the pioneers.”
The honorees this year are:
- Patricia Rice Yancy, registered nurse. Yancy, who earned master’s degrees in education and public health from UT after completing a bachelor’s degree in nursing from Mary Manse College, initiated several training courses for nurses, including critical care and flight nurse programs. She has been instrumental in training thousands of nurses, doctors and other pre-hospital employees throughout her career. She recently retired from Lourdes University.
- Patricia Ann Ambrose, paramedic. Ambrose was the EMS outreach education coordinator for Mercy Health St. Vincent Medical Center Life Flight and Mobile Life. She also was a lifelong EMS and life support educator, including playing an integral role in the paramedic education program and the former Medical University of Ohio. Ambrose died in 2018.
- Members of the Toledo Fire Department paramedic class of 1974, who are: William Brown, Michael Condon, James Dugan, David Hilton*, Alan Janney, Paul Johnston, Renzo Meraldo, James Markland, Ralph Mungons, Samuel Reynolds, Barney Rouster* and Daniel Thedford. The 1974 class was the first group of firefighters to train as paramedics in Toledo as part of a joint project with the then Medical College of Ohio. They were pioneers in their field and are uniquely responsible for building and advancing emergency medical services in Lucas County. *Posthumous recognition.
A plaque for each honoree will be added to the wall, located in the Emergency Department of The University of Toledo Medical Center, near the ambulance entrance.
UTMC, local mental health boards launch partnership to improve adolescent mental health care
Wednesday, January 16th, 2019The University of Toledo Medical Center is launching a new partnership with mental health boards throughout northwest Ohio to create a better model of care for adolescents dealing with particularly challenging mental health issues.
Through service agreements with the Mental Health & Recovery Services Board of Lucas County and 10 other boards representing 22 additional Ohio counties, UTMC will be able to provide longer, more intensive inpatient care for patients between the ages of 13 and 18.
The longer stay will enable clinicians to dig deeper into the root causes of the adolescents’ mental health issues and establish a more coordinated long-term treatment plan to address the problem of patients repeatedly going in and out of inpatient treatment without advancement.
“We want to be taking on the most difficult cases and also helping the community with its biggest needs. Right now, there’s a lot of fragmentation of services and limited access to care,” said Dr. Cheryl McCullumsmith, chair of the Department of Psychiatry at The University of Toledo. “This innovative collaboration enables an expansion of services without duplicating resources.”
In many cases, insurers will only cover a few days of inpatient treatment. While that can be enough time to stabilize many patients in crisis, some patients need a more in-depth psychiatric and medical examination, monitoring of new medications and coordination of continuing outpatient treatment, McCullumsmith said.
“There’s a high need for some adolescents to get more intensive evaluation and treatment plans,” McCullumsmith said. “We want the inpatient stay to advance the treatment plan, to be a constructive part rather than the Band-Aid it often is now. We’re trying to give them a comprehensive assessment and evaluation and kind of a restart. Let’s take some time, wipe the slate clean, start from the beginning and figure out a true diagnosis and plan.”
Under the new service agreements, the boards will pay for days not covered by insurance, allowing UTMC to treat adolescents for longer stays as needed.
The initiative will focus primarily on adolescents who have had multiple inpatient hospitalizations during the last year, have difficult to establish diagnoses or who have challenges with medication.
“We’re very excited and encouraged by the engagement with UT,” said Scott Sylak, executive director of the Mental Health and Recovery Services Board of Lucas County. “The timing was right to move forward with this and we’re really thrilled with the partnership that’s developing. Having this resource locally and being able to ensure that families stay involved and that our providers stay involved is a worthy investment from the board’s perspective.”
The Mental Health & Recovery Services Board of Lucas County, along with other partner boards across northwest Ohio, will refer patients into the program.
Founded in 1968, UTMC Child and Adolescent Psychiatry was northwest Ohio’s first hospital devoted to treating the emotional and behavioral needs of children and teens. Today, the center has an inpatient facility and outpatient mental health services.
UT engineering professors’ invention named to prestigious R&D Top 100 list
Monday, December 17th, 2018A synthetic bone graft substitute developed at The University of Toledo has been recognized by R&D Magazine as one of the year’s most exceptional innovations in science and technology.
Created by Dr. Sarit Bhaduri, Distinguished University Professor of Mechanical, Industrial and Manufacturing Engineering at UT, NovoGro is a moldable bone substitute putty used to fill gaps in bone and encourage new bone growth. It is used primarily in complicated fractures that would not otherwise heal properly on their own.
“Our composition is innovative and quite different from any of our well-known competitors,” Bhaduri said. “The response of bone growth is much faster than other products that are currently available. Our product also incorporates innovative processing techniques that simplify production, which further sets it apart.”

Dr. Anand Agarwal, left, Dr. Sarit Bhaduri, center, and Dr. Vijay K. Goel display the R&D 100 award. The three incorporated a biomedical company to commercialize Bhaduri’s invention.
R&D Magazine has annually selected the top 100 revolutionary technologies of the past year since 1963. Among this year’s other winners were Dow Chemical, Texas Instruments, the MIT Lincoln Laboratory, Oak Ridge National Laboratory and NASA’s Glenn Research Center.
“The R&D 100 Award is one of the most prestigious recognitions in applied science,” UT Vice President for Research Frank Calzonetti said. “This award speaks to the ability of Bhaduri and his University of Toledo colleagues in translating highest quality research into marketable products to improve the health outcomes of many.”
Bhaduri teamed up with Dr. Vijay K. Goel, UT Distinguished University Professor and Endowed Chair and McMaster-Gardner Professor of Orthopaedic Bioengineering, and Dr. Anand Agarwal, UT research professor of bioengineering, to license the technology from the University and co-found the biomedical firm OsteoNovus Inc. Agarwal also serves as the president and chief executive officer of OsteoNovus, where the product has undergone further development.
“In this category of orthobiologics — how to grow bone — there are many players, but the problem is the big guys aren’t doing much innovation,” Bhaduri said. “We wanted to disrupt that.”
The U.S. Food and Drug Administration has cleared NovoGro for use in two different indications — spine and the extremities.
Currently, NovoGro has a half dozen clinical users across the country and is trying to grow the client base significantly in 2019.
The company’s corporate offices and manufacturing facility is housed within The University of Toledo LaunchPad Incubation Program.
Professor awarded $2.1 million NIH grant to study fungal infection common in cancer patients
Wednesday, December 12th, 2018A University of Toledo scientist has been awarded a $2.1 million National Institutes of Health grant to continue her research into one of the most common and debilitating conditions experienced by patients undergoing treatment for head or neck cancers.
Dr. Heather Conti, UT assistant professor of biological sciences, studies a fungal infection called oral candidiasis. The infection is more commonly known as thrush.
In otherwise healthy individuals the condition is minor, but for those with compromised immune systems or undergoing radiation or chemotherapy, oral candidiasis can turn into a serious and potentially dangerous illness.
“Unfortunately, many patients who develop this condition choose to forego their cancer treatment,” Conti said. “It can actually have a direct link to cancer prognosis because the symptoms are too hard to deal with.”

Dr. Heather Conti
The five-year grant, which is distributed through the National Institute of Dental and Craniofacial Research, will fund research into the role blood platelets play in the body’s natural defense against oral candidiasis.
“Platelets are commonly thought of for their role in blood clotting. But what we’re finding more and more is that platelets also play a very important role in the immune response,” Conti said. “They can protect against various bacteria — or in our case, fungi — which is a novel thought in the field. Platelets can be a much more complicated cell than just taking part in blood clotting.”
She is collaborating with Dr. Randall Worth, associate professor of medical microbiology and immunology at UT, on the project.
The reason oral candidiasis can cause such serious problems in cancer patients is the fact that chemotherapy and radiation often destroy the mucous membrane in the mouth, allowing the fungi to grow unchecked. That, Conti said, can lead to sores on the gums or tongue, difficulty swallowing, bleeding and pain. If the fungal infection reaches the bloodstream and spreads throughout the body, it can become life threatening.
Patients with HIV are also at greater risk of serious infection from oral candidiasis.
Candidiasis can be successfully treated with antifungal medications, but Conti said there is an emerging trend of strains that have developed resistance to commonly prescribed drugs. That limits clinicians’ options, particularly in individuals who are already in poor health.
The goal of this research, Conti said, is better understanding how the body fights the infection and how we might be able to leverage that response to formulate new treatments.
“The immune response to oral candidiasis is quite complicated. If platelets play an important role, we need to understand that response. The hope would be to develop therapeutics that not only kill the fungus directly but can also bolster the immune response,” she said.
UT to host symposium on political and cultural changes brought by World War I
Wednesday, November 7th, 2018Not only did World War I reshape how modern wars would be fought, the conflict had an enormous effect on society as a whole across the globe.
“World War I was seen at the time as the ‘war to end all wars.’ It was the first global war and the first that was fought with weapons of mass destruction. It was historically important in its own right,” said Dr. Mysoon Rizk, professor of art history and director of the Roger Ray Institute for the Humanities at The University of Toledo. “But the lead up to the World War I, the absurdities on the battlefield and the war’s aftermath all brought major changes in arts, politics and culture as the world tried to make sense of the bloodshed.”
Rizk is co-organizing a UT symposium titled “Memories of World War I,” which will be held from 9 a.m. to 5 p.m. Friday, Nov. 9 in Carlson Library Room 1005.
The symposium, one of several upcoming events at UT commemorating the 100th anniversary of the Nov. 11 armistice that effectively ended the war, will bring together a diverse collection of University and community scholars to discuss the effects of the war and its cultural representations in the United States and elsewhere.
Topics to be examined include the war’s effects and consequences on Northwest Ohio and U.S. politics, the cultural memory of the war in the U.S. and abroad, how the war shaped national identities, and the innovations in art, music, literature and theater that were triggered by World War I.
Of particular note is the focus on the experiences of women during World War I.
Dr. Friederike Emonds, associate professor of German and a symposium co-organizer, said much of our contemporary understanding of the war comes from the well-known male writers of the so-called Lost Generation, while women’s war literature of the time has been overlooked.
“As women were not allowed to join the military and fight at the front, women’s war experiences offer a different perspective on the war, allowing us new insights and perceptions that significantly contribute to our efforts to gain a more comprehensive understanding of World War I today,” Emonds said.
UT has a number of other upcoming events tied to the centennial of the end of World War I, including:
- The University of Toledo Department of Theatre and Film will present an adaptation of Erich Maria Remarque’s novel “All Quiet on the Western Front.” Written and directed by Dr. Matt Foss, assistant professor of theatre at UT, the play will be performed Friday, Saturday, and Sunday, Nov. 9-11, in the Center Theatre of UT’s Center for Performing Arts.
- The University of Toledo Carlson Library will host a free screening of an English film adaptation of “All Quiet on the Western Front” from 4 to 6 p.m. on Wednesday, Nov. 14, in Room 1005.
- Through Dec. 14, the Carlson Library also is displaying World War I artifacts and photographs from the collections of Richard Oliver and the Ward M. Canaday Center for Special Collections. The exhibit is located in the library’s main lobby.
For more information on the University’s Word War I centennial events, to register for the symposium or to purchase tickets for the theater adaptation of “All Quiet on the Western Front,” visit the Roger Ray Institute for the Humanities website.
UT Pediatrics literacy program celebrates 20 years, aims to collect 20,000 books
Monday, November 5th, 2018It’s difficult to mask the clinical nature of exam rooms, even in the cheeriest of pediatrician’s offices. But a doctor’s simple gesture of handing out a storybook at every visit can make a big difference in keeping a child comfortable while providing a window into that child’s development.
During the last two decades, Reach Out and Read of Northwest Ohio — a grant-funded program of The University of Toledo Department of Pediatrics — has provided more than 258,000 books to children across the region from birth to age 5.
In honor of the initiative’s 20th anniversary, the group is in the midst of a book drive with a goal of collecting 20,000 children’s books.
“We rely on grants and donations for our entire program budget. One of our main expenses is buying books. Reach Out and Read is an important program and having community support ensures we can continue providing books that help make the experience of a doctor’s visit more child friendly, while at the same time educating parents on the importance of literacy and helping medical providers monitor development,” program director Lori LeGendre said.

UT Pediatrics residents Dr. DeAnna McGarity, left, and Dr. Rami Abdel Aziz, center, sort books with Lori LeGendre, program director of Reach Out and Read. The grant-funded program provides 28,000 books annually to area children at their pediatric wellness checks.
Reach Out and Read is an evidence-based medical model using literacy guidance as a stepping-stone to school readiness and to enhance parent-child relationships. It also serves as a literacy program, modeling the importance of reading to parents, and as a tool for pediatricians.
“Reach Out and Read is a great way for us to gauge a child’s development,” said Dr. Valarie Stricklen, a pediatrician with The University of Toledo Medical Center’s Rocket Pediatrics. “Can they point, can they name colors, can they turn pages, can they sound out words? There are many developmental milestones that we can glean from just handing them the book.”
Currently the program is at 25 sites across the region, including the Rocket Pediatrics locations in Waterville and at the Ruppert Health Center on UT’s Health Science Campus.
Reach Out and Read of Northwest Ohio serves about 14,000 children, handing out about 28,000 books a year. In some cases, the books families receive through Reach Out and Read are the only books in the home, LeGendre said.
Nationally, more than 32,000 doctors and nurses across all 50 states patriciate in the program, reaching 4.7 million children annually.
“Books are more than just reading the story and looking at the pictures. Reading is the cornerstone for language development,” Stricklen said. “That is why we give the books at six months of age before they can even talk. It teaches them the rhythm of language and speech patterns. It’s also a great way to start a bedtime routine and a way for the parent and child to connect and make reading a routine that can be fun and exciting.”
Monetary donations to the Reach Out and Read of Northwest Ohio book drive can be made by visiting Books by the Bushel. The program also is accepting donations of new and gently used books. For more information, contact Lori LeGendre at 419.291.0038 or lori.legendre@utoledo.edu. The book drive runs through Nov. 15.
UT researcher links public health of communities to likelihood of mass shootings
Wednesday, October 24th, 2018The overall public health of a community appears to correspond with the likelihood of mass shooting events, while many gun control laws do not, according to preliminary research out of The University of Toledo College of Medicine and Life Sciences.
Dr. Stephen Markowiak, a general surgery research fellow at UT, found mass shootings tend to happen more in communities that have issues with overcrowding, higher rates of income inequality, lower rates of socialization and a disconnect between mental health needs and mental health providers.
“The communities that have suffered through mass shootings tend to be much less healthy than the national average, both from a standpoint of physical health and mental health,” Markowiak said. “We need to think about this problem through the lens of public health and encourage more objective research.”
Markowiak presented his research findings Tuesday, Oct. 23, at the American College of Surgeons Clinical Congress 2018.
Dr. Stephen Markowiak
Markowiak used data from the Federal Bureau of Investigations, U.S. Census, Robert Woods Johnson Foundation and Giffords Law Center for Gun Violence to develop a slate of common characteristics of communities where 186 mass shootings have occurred.
For the purpose of the study, a mass shooting was defined as a single incident in which four or more people are killed, not including the gunman. Researchers excluded shootings that had a clear motive.
One of the intriguing findings of the research is that six of the 11 common state gun control measures Markowiak examined did not correspond with a lowered occurrence of mass shooting events. In fact, some pointed to a higher incidence.
“While the data show stricter gun control laws are associated with lower levels of overall violent crime, mass shootings appear to be the exception to the rule,” Markowiak said. “That sort of supports our notion that these are a different phenomenon than your average everyday crime.”
Five gun control measures, however, did correlate with a lower incidence of mass shootings — mandatory reporting of mental health records to the National Incident Criminal Background Check System, bans on open carrying of firearms, laws preventing child access, laws disarming dangerous persons and mandatory waiting periods.
Markowiak and research collaborators did not seek to promote any political position on gun violence but rather show it is possible to study mass shootings in a way that’s objective and apolitical.
The researchers did, however, say they believe Congress needs to take more action to ensure there is solid data available to researchers looking at the issue and to clarify that the U.S. Centers for Disease Control can investigate gun violence as a public health issue.
Although the last Congressional spending bill specified the 1996 Dickey Amendment was not an outright ban on the CDC researching gun violence as it had widely been understood, the amendment remains on the books. There’s also the so-called Tiahrt Amendment that restricts the Bureau of Alcohol, Tobacco, Firearms and Explosives from releasing much of its data to researchers.
“From a public health study standpoint, those amendments need to be revised if we’re going to ever address this issue in a more comprehensive way than we’ve done,” Markowiak said.
Co-authors include Dr. Philip Welch, assistant professor in Bowling Green State University’s Department of Public and Allied Health, and Dr. David Heidt, a trauma surgeon who formerly worked at The University of Toledo Medical Center and now works at St. Joseph Mercy Health System in Ann Arbor, Mich.

