Posts Tagged ‘The University of Toledo Medical Center (UTMC)’
UT Health physician warns allergy season extends into fall and winter
Thursday, October 27th, 2016As the warmth of early fall gives way to crisp evenings and the start of the holiday season, thoughts of raking leaves and a crackling fire come to mind. But not everyone can enjoy the crunch of drying leaves and the scent of wood burning in the fireplace.
The 30 percent of adults and 40 percent of children who are affected by nasal allergies in the United States know the sneezing, stuffy nose, sinus pressure, itchy eyes and cough of seasonal allergies are not always resolved with the change of seasons.
University of Toledo Health Allergist and Immunologist Dr. Svetlana I. Kriegel recommends those affected learn their triggers and symptoms and ways to avoid exposure to allergens to reduce the misery of nasal allergies.
“The most common are seasonal pollen allergies in the spring, summer and fall. About 70 percent of patients with spring allergies also have allergy symptoms in the fall,” Kriegel said. “We have seen a drop in temperature and with it a drop in ragweed pollen, the primary fall allergen.”
Kriegel said patients are starting to notice a change, but we aren’t out of the woods yet and other allergens, like mold are actually triggering allergic symptoms.
“The fungi take advantage of the fallen leaves and decaying vegetation this time of year and can be found in compost piles, cut grasses, wooded areas, soils, lawn debris and other moist surfaces,” Kriegel said. “In order to reduce the exposure to molds, I suggest avoiding raking leaves altogether or wearing a particle mask if you must work outside.”
A hard frost will eventually kill the foliage and bring the outdoor molds to the dormant state. However, Kriegel said indoor molds can still be troublesome, especially with humidity levels more than 50 percent. The damp air allows molds to flourish in poorly ventilated areas like attics, bathrooms, basements and under kitchen sinks.
“As we close windows and start running heaters, indoor allergens including dust mites, pets, cockroaches and molds become predominant allergy triggers,” Kriegel said. “Luckily, effective avoidance measures can diminish exposure thus decrease nasal, eye and chest symptoms. I always teach my patients this first line of defense.”
Kriegel said it is important to consider other indoor allergens as we settle in for the winter.
“As we are coming to the holiday season, we all should be jolly and happy,” she said. “Be mindful of your guests who could have an allergic or asthmatic reaction to indoor triggers.”
Smoke from fireplaces, wood burners, scented candles, air fresheners and pets can cause problems for allergy sufferers.
“If you purchase a live Christmas tree, you are at risk for carrying millions of mold spores into your home in its bark,” she said. “This mold can cause worsening of allergies and asthma in sensitive adults and kids.”
When avoidance measures are not enough to minimize suffering from allergies or when patients also experience episodic cough, wheezing or chest tightness, Kriegel develops an individualized care strategy for each patient.
“Pharmacological therapy for patients with allergies and asthma made great advances in recent years,” she said. “Medicines can significantly improve the quality of life of allergic individuals.
Nonetheless, for the most bothersome, persistent and difficult to treat symptoms, allergen immunotherapy offers a great advantage. For the right patient, allergy shots can reduce suffering from asthma and potentially cure his or her allergies.”
UT pharmacists remind patients to discuss medications during awareness month
Wednesday, October 19th, 2016Nearly half of all Americans have taken at least one prescription medication and 20 percent have used three or more prescription drugs in the last month. But according to a National Council on Patient Information and Education survey, more than half report not taking their medications as prescribed, putting them at risk for serious health concerns.
During October, which is American Pharmacists Month and Talk about Your Medicines Month, University of Toledo pharmacists are encouraging patients to build a relationship with their pharmacist in order to learn how to take medications properly, manage multiple prescriptions and reduce prescription costs.
 “Your pharmacist is likely the most accessible health care provider you have,” said Lindsey Eitniear, clinical pharmacist. “Yet not enough people take the time to talk to their pharmacist about their health. That is truly unfortunate, because we can provide many services to help our patients understand and manage their medications better.”
“Your pharmacist is likely the most accessible health care provider you have,” said Lindsey Eitniear, clinical pharmacist. “Yet not enough people take the time to talk to their pharmacist about their health. That is truly unfortunate, because we can provide many services to help our patients understand and manage their medications better.”
More than 12,000 prescriptions are filled each month across UT’s three outpatient pharmacies and pharmacists work directly with patients who are recovering in the UT Medical Center or being treated in several of UT’s clinics.
“We educate patients about taking their medication properly, identifying potential side effects and managing chronic conditions,” Eitniear said. “We also work to resolve insurance concerns and explore options for reducing out-of-pocket expenses.”
New legislation also allows a physician to permit pharmacists to make adjustments to medication dosages including those for blood pressure and diabetes at the pharmacy.
“We work closely with physicians to suggest simplifying medications or to clarify what has been ordered,” Eitniear said. “This extra communication ensures patients know how to take their medications correctly and is an added safety for patients.”
Eitniear said it is safest when patients use the same pharmacy each time they need a prescription filled, particularly if the patient takes multiple drugs.
“We can track some controlled medicines and a few others are tracked through insurance companies, but there is no one database that holds all patient prescription information,” she said. “Even a seemingly simple antibiotic can cause severe interactions with some medications. Pharmacists can spot these potential hazards if prescriptions are filled in the same location.”
Consistent use of the same pharmacy also allows a relationship to form between patient and pharmacist.
Holly Smith, UTMC Outpatient Pharmacy manager said patients should talk about all medications they are taking at each doctor’s appointment. She said printouts of all prescribed medications can be requested from the pharmacy and shared with physicians and family members.
“I tell patients to carry the list in their purse or wallet so they always have it with them,” she said. “It’s also important that there is at least one designated family member who knows your health history and medications in case of emergency.”
This also is a good time to take inventory of any leftover or expired medications. Pharmacists can advise patients the proper methods for disposing of old prescription and over the counter medications.
“We accept unwanted medications in a drop box in the emergency department of UTMC,” Smith said. “Patients with injectable medications should follow the directions on their sharps container for proper disposal.”
Smith said unused medications also can be mixed with used kitty litter or coffee grounds and disposed of in the trash. Medicated patches should be folded over and stuck together before being thrown away.
“I would advise anyone getting a prescription filled to take a minute to ask a few questions about the medication you will be taking. You can even call your usual pharmacy to review medications and discuss any concerns,” Smith said. “It is our goal as pharmacists to do the best we can by our patients so they are able to care for themselves and stay well.”
Nationally recognized expert to speak at UT lymphedema seminar
Monday, October 10th, 2016The University of Toledo’s Eleanor N. Dana Cancer Center is holding a free seminar to educate cancer patients about the latest lymphedema treatments available and provide advice for managing their symptoms.
 “Lymphedema from Head to Toe” will be held at 6 p.m. Monday, Oct., 24 at the Radisson Hotel located on The University of Toledo Health Science Campus. Registration begins at 5:30 p.m. in the Dana Cancer Center. Valet parking is available and refreshments will be provided.
“Lymphedema from Head to Toe” will be held at 6 p.m. Monday, Oct., 24 at the Radisson Hotel located on The University of Toledo Health Science Campus. Registration begins at 5:30 p.m. in the Dana Cancer Center. Valet parking is available and refreshments will be provided.
Dr. Suzie Ehmann, clinical coordinator of the edema management program at Carolinas HealthCare System, will be the keynote speaker. For more than 13 years Dr. Ehmann has dedicated her practice to the evaluation and comprehensive treatment of patients with lymphatic disorders and chronic non-healing wounds.
Lymphedema is painful swelling due to a buildup of lymphatic fluid. It is common in cancer survivors who have had lymph nodes removed or radiation therapy as a part of their treatment plan. This painful condition occurs primarily in the extremities, but also can occur in other areas of the body, such as the face and chest.
“We will review the lymphatic system and how to look for the symptoms of lymphedema,” Ehmann said. “Many patients don’t realize that occasional swelling can be the start of a much bigger problem. If we address lymphedema at this stage, it is much more treatable and improves the quality of life for patients.”
“Often lymphedema is associated with breast cancer, but those who have head and neck cancers or melanoma can also experience lymphedema,” she said.
While there is no one-size-fits all solution, Ehmann says a comprehensive treatment plan including skin care, massage, compression and exercise helps improve the quality of life of many lymphedema patients.
“This is a rare opportunity for patients and professionals alike to hear from one of the nation’s leading lymphedema experts,” said Renee Schick, event organizer and manager of UTMC’s Survivor Shop. “Anyone with a condition that can lead to chronic swelling and those who care for lymphedema patients will benefit from her presentation.”
UTMC to host community heart failure awareness symposium
Monday, October 3rd, 2016When the heart is no longer able to support the circulation of blood properly, both a patient’s quality of life and life expectancy diminishes. Heart failure patients can experience shortness of breath and fatigue, which can make everyday activities difficult.
The University of Toledo Medical Center will hold a free symposium to discuss the symptoms of heart failure, share the latest treatment options available and identify community resources available for patients.
“Navigating Heart Failure” will be 5:30-7:30 p.m. Tuesday, Oct. 11 in Room 1000A of the Collier Building on The University of Toledo Health Science Campus.
“We wanted to reach out to our community to help heart failure patients better understand their condition and the resources available to them,” said Connie Mueller, lead LVAD coordinator for UTMC and event co-organizer.
According to the American Heart Association, nearly six million Americans are living with heart failure, with more than half of them between the ages of 35 and 74. One in five people will develop the disease in their lifetime.
“People shouldn’t think of heart failure as a disease of the elderly. Young people also need to be aware of the symptoms of heart failure,” said Dr. George Moukarbel, medical director of the heart failure and LVAD programs at UTMC. “Potential warning signs are shortness of breath, increased heart rate, unusual fatigue and swelling in the extremities. The symptoms can be mild at first and often younger patients ignore or dismiss these early symptoms.”
A number of conditions can lead to the development of heart failure, including diabetes, obesity, sleep apnea and high blood pressure. Moukarbel said it is important for patients to discuss their risk of developing heart failure with their physician.
“Heart failure is a life-threatening condition with no cure, but there are treatment options available to manage symptoms and prevent further heart damage,” he said. “Medications and simple lifestyle changes can help slow the progression of the disease.”
Patients with advanced or end-stage heart failure have several treatment options available to them, including a surgically implanted pump called a left ventricular assist device, or LVAD. It is attached to the heart to help it pump more blood with less work.
“We have met with patients who were told their only remaining option was hospice care, but were able to receive an LVAD implant and are doing well today,” said Margaret Commet, operations supervisor of UTMC’s cardiovascular unit and event co-organizer. “It is important that heart failure patients understand that advanced treatments can give them more time and improve their quality of life.”
With his heart functioning at only 10 percent, Byron Clark was given only six months to live in early 2015.
“I decided to get the LVAD implant at that time because I didn’t think six months was long enough to wait on the transplant list,” said Clark, who had the LVAD implanted at UTMC. “It did take some adjustments to learn to live with the implant, but it gave me time until a donor was found 16 months later.”
“For patients like Byron, the LVAD is a bridge to transplantation,” said Dr. Mark Bonnell, UTMC cardiothoracic surgeon and director of the LVAD program. “Others who are not eligible for a transplant can still see a substantial improvement in quality of life from LVAD as a permanent solution. The LVAD has added not only years but quality to their lives which is indeed the central purpose of this technology.”
More than 18,000 patients worldwide and 39 patients at UTMC have received implantation of the LVAD device.
“I definitely recommend having the LVAD implant and the doctors at UTMC,” Clark said. “It gave me extra time and I feel great today. My new heart is functioning well and I look forward to working in the yard and traveling.”
Clark and his wife have established the Having a Heart for a Heart Foundation to educate and guide families through the LVAD to transplant process and provide financial support for patients.
“We were blessed to have good insurance, but we know others who have lost everything trying to manage the financial burden of these surgeries,” said Debbie Clark, foundation president. “We wanted to do something to give back and help others who need to travel this journey.”
Dr. Moukarbel and Dr. Bonnell will speak at the “Navigating Heart Failure” event, along with patients who will share their experiences in living with heart failure. Vendors and educational booths will be available, including information about cardiac rehab, smoking cessation, respiratory therapy and proper nutrition.
Preregistration is required. Call 419.383.5150 by Thursday, Oct. 6 to register. Nurses can earn one continuing education credit for attending.
UT Health hosts free wellness expo
Monday, October 3rd, 2016To promote healthy living in northwest Ohio, University of Toledo Health will hold a free Wellness Expo 9 a.m. to 2 p.m. Saturday, Oct. 8 at Glendale Medical East, 3333 Glendale Ave., Toledo.
 Local health experts will present information on a variety of topics including the effects of physical activity in the prevention of diabetes, how stress and depression play a role in cardiac disease, care for expectant mothers and Lucas County Health assessment data.
Local health experts will present information on a variety of topics including the effects of physical activity in the prevention of diabetes, how stress and depression play a role in cardiac disease, care for expectant mothers and Lucas County Health assessment data.
Attendees will have access to free health screenings including blood glucose, blood pressure, lung capacity and HIV testing. Flu shots also will be administered at the event.
“We want to empower individuals in northwest Ohio to take charge of their own wellness and are pleased to provide this opportunity to share important health information to the members of our community,” said Dr. Johnnie Early, event organizer and dean of the College of Pharmacy and Pharmaceutical Sciences.
Vendors will share information about smoking cessation, managing blood pressure, preparing healthy meals, asthma control and heart health. Representatives from Life Connection of Northwest Ohio, the American Heart Association, Lucas County Children Services and other community resource organizations will also be on hand to share information about their services.
Visit http://uthealth.utoledo.edu/webforms/health-expo.html or call 419.383.1904 to pre-register.
Three selected for UT’s Emergency Medicine Wall of Honor
Tuesday, September 27th, 2016The University of Toledo Medical Center will recognize three individuals for their contributions to the field of emergency medical services at the Emergency Medicine Wall of Honor Ceremony.
A reception will start at 11:30 a.m. on Tuesday, Sept. 27 in the Jacobs Interprofessional Immersive Simulation Center on the Health Science Campus. The program begins at noon with remarks from UT President Sharon L. Gaber, Dr. Christopher Cooper, executive vice president for Clinical Affairs and dean of the College of Medicine and Life Sciences, and Dr. Kristopher Brickman, professor and chair of the Department of Emergency Medicine.
“This is the sixth year we have honored those who have made a significant contribution to the field of emergency medicine,” Brickman said. “The individuals recognized are the trailblazers in their field and they have set the gold standard for what it means to be an emergency medicine professional.”
The Emergency Medicine Wall of Honor, made possible through funding from The Blade, was established in 2011 to celebrate the achievements of those who have lived a life of self-sacrifice in committed service to the emergency medicine community.
Each year, nominations are submitted by a committee of community stakeholders and reviewed by a multidisciplinary selection committee.
This year’s honorees are:
- Carl W. Neeb, retired Toledo Fire Chief. After serving 30 years with the Toledo Department of Fire and Rescue, Neeb retired as chief of the department in 1980. He was known as the “Father of Paramedics” in Toledo due to his invaluable contributions in establishing emergency medical services within the Toledo Fire Department. His expertise and involvement helped develop and implement Lucas County’s Advanced Life Support System and was instrumental in its success as one of the first and finest systems in the country.
- Bruce D. Janiak, professor of emergency medicine, Medical College of Georgia. Janiak was the first resident in emergency medicine in the United States and is recognized as one of the fathers of the specialty. He is considered a true visionary in the field, having explored and implemented concepts such as telemedicine well before it became standard practice. He served as president of the American College of Emergency Physicians and the Emergency Department Benchmarking Alliance, an organization that defines the best clinical and administrative practices. He is a lecturer, instructor and author and consultant specializing in medical malpractice.
- Judith A. Ruple, registered nurse. Ruple was chair of the National Emergency Cardiovascular Care Committee Education Subcommittee for the American Heart Association and president of the National Association of EMS Educators. She was the director of the Emergency Medical Technician-Paramedic program in the UT Department of Health and Human Services. Ruple served as a content level leader of the National EMS Education Standards Project and was the principal investigator for the State of EMS Education Research Project, funded by the U.S. Department of Transportation. She has written more than 35 publications and received numerous grants for research and development in the area of Emergency Medicine Services Education.
Ryan White Program hosts inaugural event to support HIV/AIDS community
Tuesday, September 27th, 2016Ryan White Program hosts inaugural event to support HIV/AIDS community
The University of Toledo Medical Center’s Ryan White Program will host a night of dinner and dancing to support HIV and AIDS patients and their families.
“Re-tie the Red Ribbon” is Saturday, Oct. 1 from 6-10 p.m. at Hensville in downtown Toledo. Tickets are $50 each and include a variety of food stations and live entertainment by Fu5ion.
“We are excited to kick off this brand new event in such a great venue,” said Richard Meeker, manager of 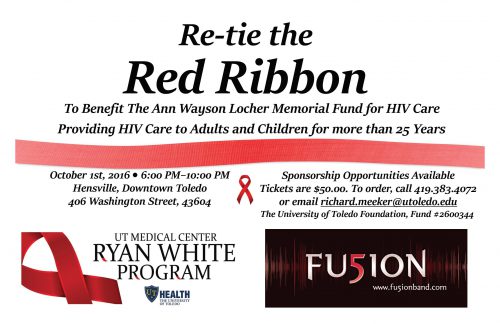 fundraising and special projects for the Ryan White Program. “The funds we raise will go to the Ann Wayson Locher Memorial Fund for HIV Care to provide support to adults and children in the Toledo area affected by HIV.”
fundraising and special projects for the Ryan White Program. “The funds we raise will go to the Ann Wayson Locher Memorial Fund for HIV Care to provide support to adults and children in the Toledo area affected by HIV.”
Ann Wayson Locher opened the first grant-funded free and anonymous HIV testing site in northwest Ohio in 1985 and was one of the key organizers of the Ryan White Program.
Her daughter said she was an infection control nurse who was passionate about caring for those in underserved populations.
“She focused in on HIV care in the 1980s and never looked back,” Megan Locher said. “My siblings and I grew up in the clinic and as we got older we all volunteered there. The physicians, nurses and staff became members of our family. We learned the importance of giving back to the community and caring for those who were struggling.”
The Ann Wayson Locher Memorial Fund was created in her honor upon her death in 2010. The fund continues the work she started and provides health care and social services for HIV and AIDS patients who have needs that cannot be covered by other agencies or programs.
“She was passionate about identifying gaps in health care and finding ways to reach those who needed help the most,” her daughter said. “She didn’t want patients to have to choose which health care services they could receive based on their financial or personal situation.”
Meeker said the organization has seen an increase in the number of clients seeking assistance.
“The number of families requesting assistance for housing and basic living assistance has been on the rise in recent years,” he said. “The goals of this event are to enlist the community in supporting these families and to raise awareness of HIV and AIDS in Toledo and northwest Ohio.”
UTMC’s Ryan White Program uses a multidisciplinary approach to provide health care services and support to persons living with HIV and AIDS in the Toledo area. It is the regional referral center for patients needing assistance.
“Mom and her team developed the program to be a place where people could get comprehensive care,” Megan Locher said. “The team is made up of a dedicated group of physicians, nurses, nutritionists, social workers and financial counselors and so many more professionals who work tirelessly to provide a network of care to HIV and AIDS patients and their families. Her legacy lives on in the lives that continue to be improved through the services the Ryan White Program provides.”
Call 419.383.4072 or email Richard.Meeker@utoledo.edu to order tickets.
UT physician warns overloaded backpacks could cause health problems
Tuesday, September 20th, 2016School is in full swing and that means backpacks are loaded with textbooks, binders, homework and athletic gear. Backpacks are convenient for toting must-have items to school, but they can quickly become too heavy for children to carry safely.
Sept. 21 is National Backpack Awareness Day and a University of Toledo physician advises parents to make sure children are properly  loading and carrying backpacks to avoid back strain and pain.
loading and carrying backpacks to avoid back strain and pain.
“When a backpack is too heavy, its weight can pull the child backwards,” said Dr. Nabil Ebraheim, professor and chair of the Department of Orthopedic Surgery. “The child counteracts the weight by arching their back or bending forward, causing the spine to compress unnaturally, which can contribute to neck, shoulder and back pain.”
The best way to avoid back strain is to avoid overloading backpacks. According to the American Academy of Orthopedic Surgeons, children should limit their backpack weight to between 10 and 15 percent of their body weight.
“It also is important that backpacks are sized properly to the child and have wide, padded straps as not to restrict circulation or cause nerve pain,” Ebraheim said. “A backpack with a waist strap also may help to transfer weight to the hips and help to prevent slouching.”
Students should be taught how to properly carry a backpack to avoid serious injury or long-term damage to the spine.
“Carrying a backpack over just one shoulder causes an uneven distribution of weight that forces the child to compensate by leaning to one side,” Ebraheim said. “That causes muscle strain and extra stress on the discs in the spine. Over time it could contribute to more serious back problems such as scoliosis.”
Ebraheim said when loading a backpack, try to concentrate the bulk of the weight closest to the child’s body and near the middle of the back. This distribution of weight will help the child achieve better posture and balance, reducing the risk of back or neck injury and falls.
He said schools who are replacing heavy textbooks with tablets are on the right track.
“With today’s modern technology, there’s no reason students should be carrying so many textbooks back and forth to school,” he said. “Schools that make the switch to digital learning are doing more than simply engaging students with an interactive way to teach, they also are protecting students’ health by lightening the load of their backpacks.”
UT physician recommends specialized care for senior citizens
Wednesday, September 14th, 2016Aging is inevitable and health issues can start to arise as our bodies get older. While some aches, pains and forgetfulness are a normal part of this process, other symptoms can signal a more serious problem.
September is Healthy Aging Month and UT Health physicians want to remind caregivers that now is a great time to take a closer look at the health of the senior citizens in their lives.
“When most people think of health care concerns as we age, they most commonly think about memory loss and dementia. It is a major concern because it limits the physical, mental and financial independence of the elderly,” said Dr. Anu Garg, program director of the Geriatric Medicine Fellowship. “It’s important that seniors and their families seek out care early. We can help to maintain their quality of life longer.”
Darletta Snyder said she sought out a geriatrician when she felt her husband’s needs were no longer a good fit for their family practice physician.
“Sam had some concerns about his memory and I thought it would be best if we found a doctor that was specially trained in caring for us,” she said. “Dr. Garg listened to our concerns and felt it would be a good idea to have a more detailed evaluation done. Everything came out fine for Sam, but she has continued to care for us and does a great job in seeing we stay healthy.”
Garg said warning signs of dementia can include repeating questions, forgetting to pay bills or take medications and leaving the stove or oven on.
“As we age, we do become more forgetful, but this forgetfulness should be seen as a warning sign and the patient should be evaluated,” she said. “We use the St. Louis University Mental Status (SLUMS) evaluation to determine if there are signs of early dementia and can start medications that can slow its progression, if necessary.”
Garg said there isn’t a cure for dementia or Alzheimer’s disease at this time, but she has begun collaborating with a UT assistant professor of neuroscience to explore new medications for treatment.
Dr. Joshua Park received two grants this year to assist in funding his research into how a common food additive could reverse brain cell damage caused by the disease. Midi-GAGR, a byproduct of low acyl gellan gum, has already shown promise in lab testing to reverse the effects of Alzheimer’s disease in mice.
“There is still much more testing to do before we will be approved for human trials, but it should move fairly quickly as low acyl gellan gum is used as a thickening agent in foods like pudding and has already been approved for human consumption by the FDA,” he said.
Until a cure is found, patients and their caregivers need to know there are support systems available for individuals who are experiencing memory loss and early symptoms of dementia.
“This is a progressive disease and it can become very difficult for caregivers to support their loved one as they become less independent,” Garg said. “We work with social workers to reach out to organizations and programs and connect them to families as they travel this path.”
Social workers connect patients with community resources such as the Alzheimer’s Association, Area Office on Aging and Lutheran Village at Wolf Creek which provide geriatric wellness and caregiver support programming.
UT’s Center for Successful Aging is another resource for education and finding resources within the community.
“Our focus is on education, research and service,” said Victoria Steiner, assistant director of the Center. “We offer a graduate certificate in gerontology to support those who wish to work with seniors, participate in local research to determine our community’s needs, and work closely with area support organizations to provide educational outreach programs and to connect individuals with the support they need to age well.”
Garg created a support fund for the Center to continue to promote geriatric medicine education for students, residents and fellows, enhance research activities and education activities, and promote teambuilding and support activities for those who provide senior care.
“It is important that all caregivers, including medical team members, take time to get the support they need when caring for elderly patients,” she said. “It can be very taxing as patients can progressively lose their independence and it’s easy to get burnt out.”
While caring for aging patients can be challenging at times, Garg said she is confident she is making a difference for older adults and their families.
“Going to see Dr. Garg is enjoyable,” Snyder said. “She is very knowledgeable and listens to us and has a great sense of humor. It’s comforting to know we are with someone who cares and stays on top of our health.”
UT to hold seminar on prostate cancer and urological health
Monday, September 12th, 2016Surgery and radiation therapy for prostate cancer can cause undesirable side effects for men including erectile dysfunction and incontinence, but a cancer diagnosis does not mean a man’s quality of life needs to suffer.
A seminar aimed at educating men about available options for prostate cancer and improving their overall urological health will be held 6 p.m. Thursday, Sept. 15 at UT Health’s Eleanor N. Dana Cancer Center. Registration begins at 5:30 p.m.
“It is important for men who are diagnosed with prostate cancer to ask about the treatment options that are available to them,” said Dr. Samay Jain, UT Health vice chief of staff and division chief of urologic oncology. “Men with low-risk prostate cancer may be good candidates for active surveillance, which means we monitor him closely, but delay surgery or radiation treatment until it is needed.”
If active treatment cannot be avoided, Jain says there are options to help preserve a man’s quality of life.
“Our surgeons are trained in robotic surgery and other minimally-invasive therapies for the cure of prostate cancer to help you get back to living your life with less pain and scarring and reduced risk of side effects,” he said.
Jain encourages men experiencing incontinence or impotence to talk to their doctor about the treatment options available including medications, therapies and surgical options.
“Shifting Focus: Thinking Beyond Prostate Cancer and into Survivorship” is part of the Eleanor N. Dana Cancer Center’s Wellness Information Series. Jain is certified through the American Board of Urology and focuses on urologic oncology, minimally invasive robotic procedures and prostate MRI.
Space is limited and reservations are required. Email EleanorNDanaCancer@utoledo.edu or call 419.383.5243.



